A 24 YEAR OLD MALE WITH HEMATEMESIS
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
HISTORY OF PRESENTING ILLNESS:
A 24 year old male, from Chitavaram, carpenter by occupation, presented with the complaints of 2 episodes of bloody vomiting and chest pain since 1 day.
The patient was apparently asymptomatic 2 days ago. He then consumed alcohol from morning to night for the whole day without consuming any food. He started vomiting at night and his vomit contained blood, it was non bilious and non projectile in nature. Following vomiting episodes he became unconscious. He was brought to the hospital post mid night between 1 and 2am. He also complained of chest pain which started following vomiting and it was pricking type of pain which was continuous in nature and present in the mid area of chest.
PAST HISTORY:
There were no similar complaints in the past.
Patient started consuming alcohol 6 years ago with his friends and from then he started drinking alcohol (whisky) 180ml daily which gradually increased to 540ml as he is not getting the same high as before. He also started chewing tobacco around the same time and consumes about 2 packs daily since 4 years. The patients abstains from alcohol for 2 months in an year for religious purposes during which he experiences symptoms such as tremors and sleep disturbances.
No history of Diabetes, Hypertension, TB, Asthma, Epilepsy, CAD, CVA
PERSONAL HISTORY:
GENERAL EXAMINATION
Patient is conscious, coherent, well oriented towards time, place and person.
Pallor - absent
Icterus - Mild
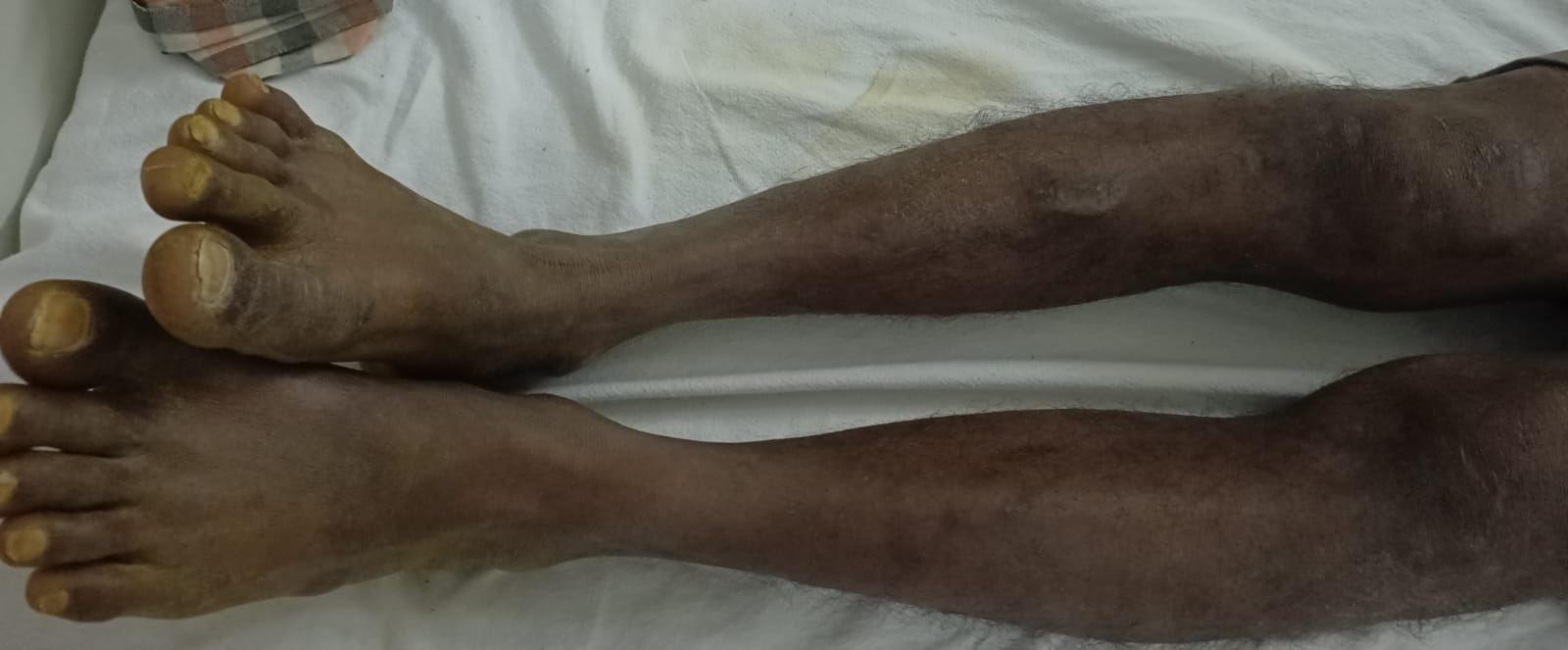
Clubbing-absent
Cyanosis-absent
Lymphadenopathy - absent
Edema-absent
VITALS
Temperature- afebrile
Pulse rate - 84 bpm
Respiratory rate- 16 bpm
Bp-120/80
SYSTEMIC EXAMINATION







Comments
Post a Comment