70 year old female with lower back pain
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE
This is a case of a 70 year old female admitted in the ward, with the complaints of:-
Lower back pain since 2 days
Low grade fever since 10 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 20 years ago. She had a history of giddiness and consulted a physician following which she was diagnosed with hypertension and was started on Tab Atenolol.
The patient presented to the causality 4 years ago with pain in right hip and was unable to walk due to fall from an auto following which she was was diagnosed with right femur fracture and operated in our hospital. Proximal femoral nail was used for fixation.
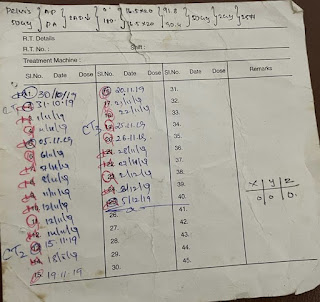
3 1/2 years ago she developed bleeding with white discharge per vagina and came to OBG department for checkup. She was diagnosed with carcinoma of cervix II B and she underwent radiotherapy at MNJ for 5 weeks in November to December 2019 a total of 25 sessions.
On 7th November she presented with abdominal pain in the left upper quadrant, which was relieved on vomiting. The vomiting occurs a few hours after eating. The vomit consisted of the food she consumed which is not foul smelling or blood stained and non bilious. She was diagnosed with acid peptic disease. On investigation she was diagnosed incidentally with severe anemia with a haemoglobin of 4gm/dl for which she had blood transfusion on 11th November and she was discharged on 16th November. Investigations also relieved pernicious anemia.
On 23rd November , she came to opd with lower back pain since 2 days, associated with fever since 1 week. The pain is continuous, dull aching type, radiating to groin, no tenderness, no history of tingling or numbness. There are no aggravating factors and the pain is temporarily relieved on medication.
The fever is insidious in onset, gradually progressive, associated with 3 episodes of nausea and vomiting
PAST HISTORY:-
20 years ago she was diagnosed with hypertension and treated with Atenolol.
4 years back she had proximal femur nail operation for femur fracture.
No history diabetes mellitus, epilepsy, TB, asthma, thyroid abnormalities.
PERSONAL HISTORY:-
She has one daughter and lives with her.
She worked in a school as aaya for 23 years.
She usually used to wake up at 6 AM in the morning, but from past few months she wakes up at 8 AM stating lack of energy.
Usually after waking up she used to do all the household work such as cleaning, washing the utensils, etc.
She consumed breakfast like idli, dosa, Upma, etc. at around 7AM and went to school by 8AM.
She usually packs lunch for herself from home and consumes at 2 PM.
She used to come back from school by 6 PM finish her household work and cook dinner, which includes rice with curry and took bath and slept by 9PM.
She consumes diet rich in carbohydrates like rice , etc and consumes both veg and non veg food.
She consumes tea 3 times per day every day.
Currently she mostly rests at home due to lack of energy. Her appetite has decreased which leads to irregular bowel and bladder movements. She didn’t defecate properly from the past 3 days.
She has no addictions.
There is no history of allergy.
TREATMENT HISTORY:-
Tab. Atenolol for hypertension.
Chemo radiation 4 years ago for 5 weeks for the treatment of Cervical carcinoma stage IIB
She had blood transfusion for severe anemia
FAMILY HISTORY:-
No similar complaints in the family.
GENERAL EXAMINATION:-
Patient is conscious, coherent, uncooperative
Well oriented to time, place and person
Thinly built and moderately nourishment.
VITALS :-
Temp - afebrile
BP - 130/90 mm/hg
Pulse rate - 86 bpm
Respiratory rate - 13 cycles per minute
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Oedema - absent
SYSTEMIC EXAMINATION
CVS
S1 S2 heard
Murmur heard in aortic area.
RESPIRATORY
- Chest bilaterally symmetrical, all quadrants
moves equally with respiration.
- Trachea central, chest expansion normal.
- Resonant.
- Bilateral equal air entry, no added sounds heard.
CNS
GCS - 15/15
- No focal neurological defects
- All cranial neves are intact.
Higher mental functions intact
Power:-
Rt UL-5/5. Lt UL-5/5
Rt LL-5/5. Lt LL-5/5
Tone:-
Rt UL -N
Lt UL-N
Rt LL-N
Lt LL-N
Reflexes: Right Left.
Biceps. ++. ++
Triceps. ++ ++
Supinator. ++ ++
Knee. ++ ++
Ankle. ++ ++
Plantar: Flexion Flexion
P/A
Abdomen is soft and non tender
No organomegaly
Bowel sounds heard
No shifting dullness or fluid thrill
PROVISIONAL DIAGNOSIS
Fever under evaluation
Lumbar Spondylosis
Pernicious anemia
Hypertension
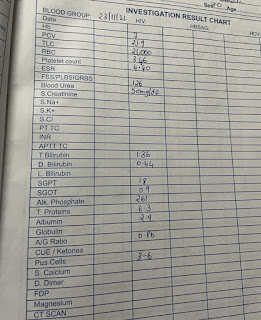
INVESTIGATIONS
ECG
Echo
AP VIEW
Laboratory investigations















Comments
Post a Comment