Case Based OSCE Along With Bloom's Learning Levels Achieved
Case Based OSCE Along with Bloom's Learning Levels Achieved
Note - This is an a online e log book to discuss our patient's de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment
CHIEF COMPLAINTS:
The patient presented to the OPD with the chief complaints of -
- Lower abdominal pain since 10 days
- Bilateral pedal edema since 3 years
HOPI:
The patient was apparently asymptomatic 10 days ago and then he developed pain in the lower abdomen which is sudden in onset, non radiating, dragging type, no aggravating factors, relieved temporarily on medication.
The patient also complains of bilateral pedal edema of pitting type since 3 years which occurs on prolonged sitting and relieved at night on lying down in supine position with legs elevated. The patient also mentions that he urinates 2 to 3 times during the night following which the pedal edema is relieved. This urge to urinate multiple times at night leads to disturbance in his sleep.
No h/o SOB, orthopnea, PND, palpitations, giddiness, fever, diarrhea, constipation, lower urinary tract symptoms, discolorations of urine or stools, bleeding manifestations
PAST HISTORY:
K/c/o Hypertension since 5 years, using Amlodipine 5mg and Atenolol 50mg
Pt complained of pain in right upper abdomen 7 years ago and was diagnosed with Cholelithiasis, underwent Cholecystectomy
N/k/c/o DM, Asthma, TB, Epilepsy, CAD, CVD
PERSONAL HISTORY:
The patient wakes up at 5:00am and finishes his morning chores such as brushing, bathing and breakfast. His occupation is animal husbandry and business involving farm animals. His job involves him travelling often on the bike and in the bus during which his pedal edema is exacerbated. He sleeps at around 9:00pm daily. His sleep is disturbed due to urge to urinate multiple times during the night.
His diet is mixed, appetite is normal and bowel and bladder movements are regular
GENERAL EXAMINATION
Patient is conscious, coherent and cooperative and well oriented to time, place and person
He is well-built and nourished
No pallor, icterus, cyanosis, clubbing, lymphadenopathy and pedal edema
Vitals on admission -
Temp - Afebrile
BP - 120/80 mm hg
PR - 78bpm
RR- 18cpm
SYSTEMIC EXAMINATION:
CVS: S1, S2 heard , no murmurs
CNS: NAD
RS: B/L air entry + , trachea central , NVBS heard
P/A : obese, midline scar present, soft, non tender
Splenomegaly present, spleen palpable 4-5cm below the costochondral margin.
PROVISIONAL DIAGNOSIS:
?Tropical Splenomegaly
TREATMENT:
Inj ARTESUNATE 180mg
Inj MULTIVITAMIN 1amp in 100ml NS OD
Tab SHELCAL PO/OD
Bloom's Taxonomy levels:
1. Knowledge (Remembering):
Tropical splenomegaly syndrome, also known as hyperreactive malarial splenomegaly, occurs due immunological overstimulation to repeated attacks of malarial infection over a long period of time.[1] Condition is usually seen in malaria-endemic areas like Africa and Indian subcontinent.[2] Tropical Splenomegaly Syndrome is characterized by massive splenomegaly, hepatomegaly, marked elevations in levels of serum IgM and anti-malarial antibodies. The spleen is massively enlarged. It shows dilated sinusoids lined with reticulum cells. There is a marked erythrophagocytosis and lymphocytic infiltration of the pulp. Peripheral smear for malarial parasite is usually negative.
2. Comprehension (Understanding):
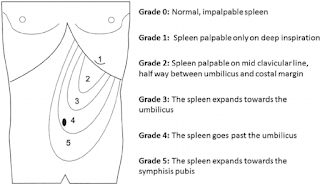
GRADING OF SPLENOMEGALY
SOURCE:- https://images.app.goo.gl/dGDzDfVa6G7qYnas7
CRITERIA FOR SPLENOMEGALY
SOURCE :- https://images.app.goo.gl/Ai9Zx2FJvfvRZnvZ9
3. Application (Applying):
Medical Care
Therapy is based on the use of antimalarial drugs. A literature review by Leoni et al indicated that a short therapy course is sufficient treatment for HMS in patients who, after exposure to malaria parasites, do not revisit areas where malaria is endemic. In such patients, according to the study, elimination of the infection effectively cures the splenomegaly. The investigators, who drew data from 89 papers, asserted that patients who continue to be exposed to malaria-endemic regions require intermittent therapy or possibly lifelong treatment. [34] Addition of doxyxline to the antimalarial may be of benefit; Genderini et al administered dihydroartemisinin/piperaquine (320/40 mg three tablets/day for 3 days) with doxycycline 200 mg to a patient once a day for 6 weeks, with complete resolution of HMS.
A retrospective, longitudinal study by Bisoffi et al indicated that patients with early HMS should receive the same treatment as patients with the full-blown syndrome, since early HMS predisposes patients to the more advanced condition. The study found that among patients with early HMS, re-exposure to malaria is a major risk factor for progression and stated that, while a single antimalarial treatment will probably prove adequate against early HMS, antimalarial prophylaxis should subsequently be used in re-exposed patients.
Surgical Care
Splenectomy plays no role in the treatment of hyper-reactive malarial splenomegaly (HMS) and should be avoided, as it can result in fulminant and overwhelming infections with high mortality.
SOURCE :- https://emedicine.medscape.com/article/959720-treatment?form=fpf
4. Analysis (Analyzing):
l MP STRIP TEST - NEGATIVE
l USG ABDOMEN - POST CHOLECYSTECTOMY STATUS, B/L GRADE 2 RPD CHANGES WITH RENAL CORTICAL CYSTS, GROSS SPLENOMEGALY
l LIVER FUNCTION TEST:- T.B:- 1.45 DB :-0.42 AST:-14 ALT 16ALP:- 104 T.P :- 6.0 ALBUMIN:-4.35 A/G RATIO :- 2.64
l RENAL FUNCTION TEST:- UREA :- 27 CREATININE : 0.9 URIC ACID :- 5.7 CA2+ :- 9.5 PHOSPHORUS:- 2.7 NA+/K+/CL- : - 136/3.6/101
l COMPLETE URINE EXAMINATION :- NORMAL
l HEMOGRAM
HB:- 12.2
TC:-4,700 N/L/E/M/B :- 63/29/02/06/00
PCV/MCV/MCH/ MCHC :- 32.8/79.2/29.5/37.2
RBC COUNT:- 4.14
IMPRESSSION:- NORMOCYTIC NORMOCHROMIC BLOOD PICTURE WITH MILDHYPOTHROMBOCYTOPENIA
5. synthesis (Creating):
SO WE FOLLOWED BELOW TREATMENT PLAN FOR 5 DAYS
l Inj. ARTESUNATE 180mg
l Inj. MULTIVITAMIN 1amp in 100ml NS OD
l Tab SHELCAL PO/OD
6. Evaluation (Evaluating):
WE GAVE ARTESUNATE 180mg/I.V for 5 days after which pt. Complaints were relieved and hence was discharged in HEMODYNAMICALLY STABLE CONDITIONS .


Comments
Post a Comment